Recently I was asked to contribute to an article on prolapse, and due to word count restrictions, all the information I wanted to share couldn’t be included, so I thought I would do a post!
Prolapse after pregnancy and birth is common, with approximately 50 percent of women experiencing some type of prolapse; depending on the cause, the symptoms can be subtle or demand your attention. However, we mustn’t normalise the symptoms as just a part of postpartum. Early assessment and management by a health care professional and physiotherapist are vital in alleviating symptoms and slowing prolapse progression.
So why is prolapse so common?
During pregnancy, the pelvic floor may be weakened due to hormone changes and the weight increase, and then during birth, prolonged pushing and tears or a bigger baby can also contribute.
Additionally, your personal and medical history can contribute to your increased risk of prolapse, including:
- Family history of vaginal prolapse and a personal history of previous prolapse
- Previous prolapse repair
- Conditions that cause prolonged coughing – asthma, bronchitis, smoking
- Constipation – straining to have a bowel motion
- Lifting heavy things regularly – including older children
- Being overweight
- Pelvic tumour or fibroids
- Going through menopause – low oestrogen levels lead to muscle laxity
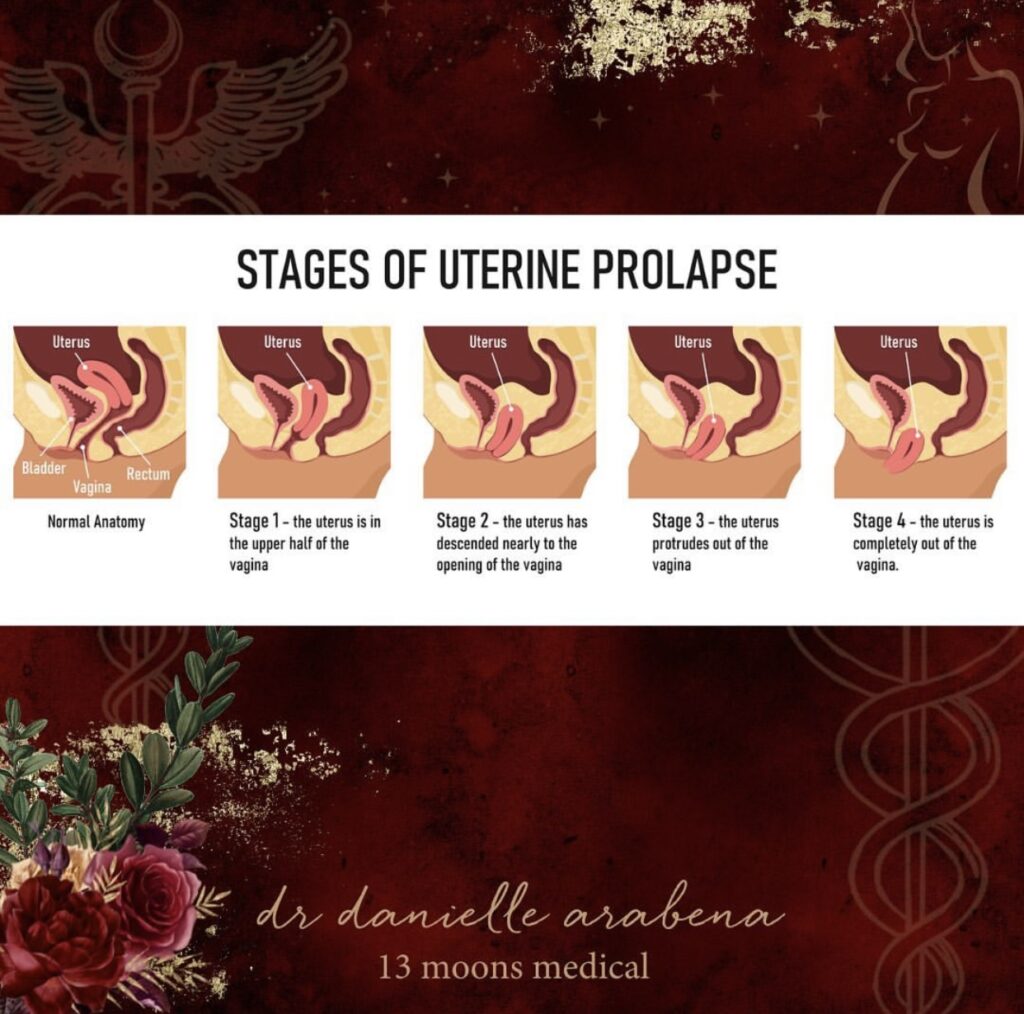
Most early-stage prolapses are noted during cervical screening tests, but as the prolapse progresses, we start seeing more symptoms ( again, that can get overlooked), including:
- Achy pain in the pelvic and lower back region
- A sensation of heaviness or dragging, mainly after coughing or standing for a long time
- You may see or feel a lump inside your vagina or just outside
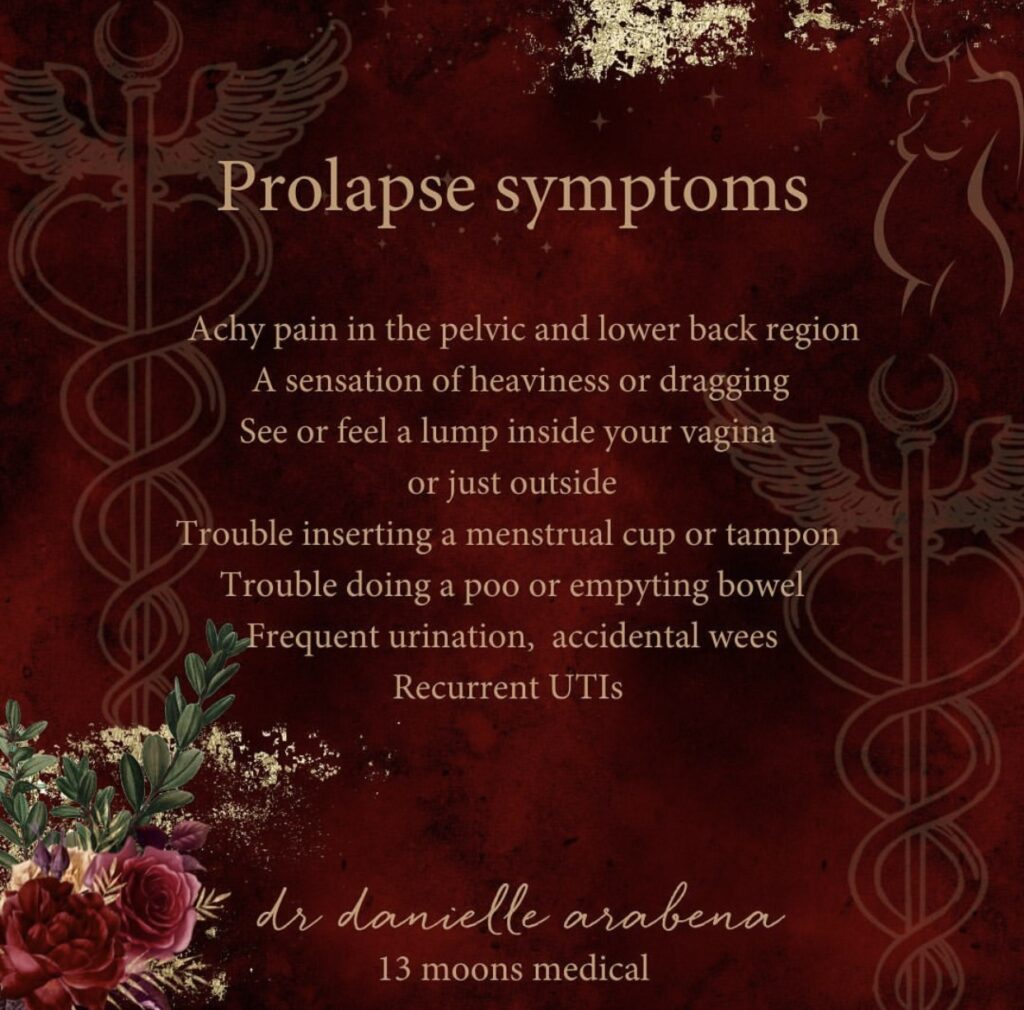
The pelvic floor is responsible for keeping your uterus in place and supporting the bladder and your bowel. So when there is a weakening of the pelvic floor, you can get prolapses of the bladder and bowel, resulting in changes in how you go to the toilet. As a result, some people can experience needing to wee a lot, weeing accidentally, and recurrent UTIs, or they may have trouble emptying the bowel.
How is prolapse treated?
Well, this depends on what organ has prolapsed and how far ( what stage it is at), how old you are, your health and whether you want more children.
An excellent place to start is lifestyle changes that can prevent prolapse or stop it from getting worse, including quitting smoking, losing weight, managing your cough, and trying to lift less.
Get your multidisciplinary treatment team on board. For example, besides seeing a Doctor, a good women’s health physiotherapist will access & make recommendations for a unique pelvic exercise plan – doing Kegels too often or incorrectly can fatigue your pelvic floor muscles.
A stabilising device like a pessary may reduce symptoms and improve your quality of life; a repair to the pelvic floor will need surgery.
Treatments that balance the physical & energetics of the womb space /pelvic bowl, like holistic pelvic care, can help with symptoms – particularly in the earlier stages. In addition, this type of work can allow for healing and a deep connection to the pelvic floor, and I often find women will have a much-needed emotional release during the treatment.
In these treatments, there is an assessment followed by techniques like intervaginal massage with myofascial release and trigger point work, as well as breathwork and visualisation tools to help restore physical and energetic balance.
Not all of these treatments are successful, and prolapses can reoccur
So if you have any of these risk factors and sense a feeling of something not being right down there, PLEASE get a review.